2024 Hope Newsletters
July 2024
Opioid Stewardship Management Plans: Due October 1, 2024
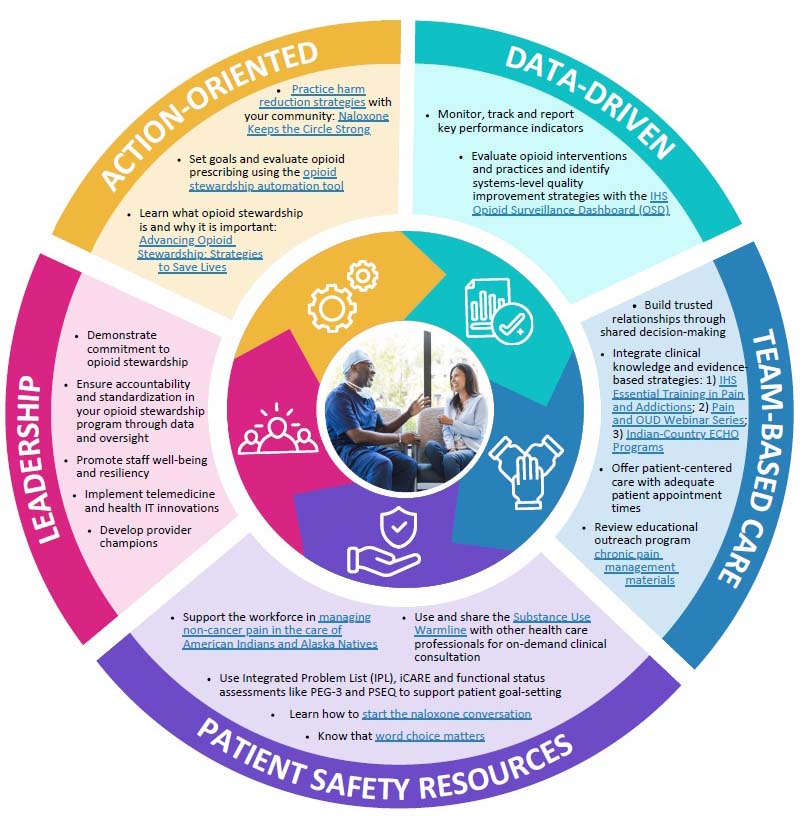
An IHS SGM was released to promote the safe and effective use of opioids through the creation and maintenance of mandatory Opioid Stewardship (OS) Management Plans, which are due October 1st and should be updated at least every two years. Consider using the IHS OS automation tool designed to assist sites and committees with an evaluation of current opioid prescribing practices and facilitate discussion surrounding opportunities for improvement. The interactive tool will guide team discussions as users consider core elements of OS programs.
Utilizing the tool will result in an OS management plan customized to your local facility!
- Visit the opioids website for more information.
- For details, consider reviewing the SGM.
- The OS infographic is available for download!
IHS Pain and Opioid Use Disorder Webinar: Advancing Opioid Stewardship - Leveraging Local Strategies and other webinars are available!
Reversing Opioid Overdose with Naloxone Training: Due December 31st
All IHS federal employees, contractors, and clinical residents must complete this training course annually. It consists of three short videos:- Risk factors for overdose and signs/symptoms of opioid overdose
- Best practices for administering naloxone
- Identifying naloxone storage location (if applicable) and ways to obtain naloxone
Contractors, interns, and intermittent employees must complete the training via course material and present the passing certificate to their contract lead or supervisor.
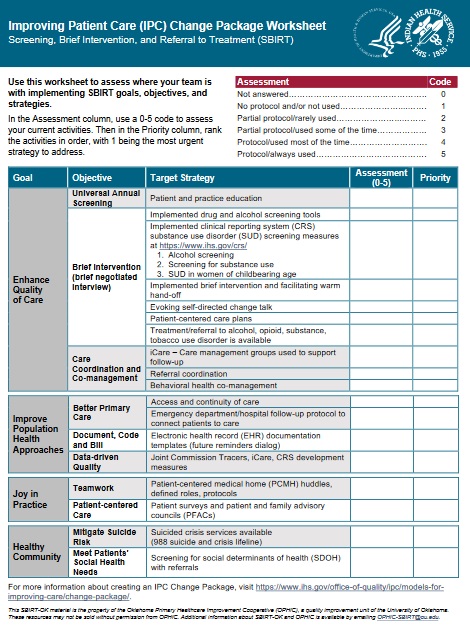
Drug and Alcohol Screening: SBIRT, TAPS, and CAGE-AID Tools
IHS is expanding education and outreach that utilizes evidence-based approaches to substance use disorder (SUD) care which includes enhanced universal screening and care-coordination efforts that support patient engagement and reduce opioid overdose rates.Steps to improve screening at your facility
- Complete the Improving Patient Care (IPC) Change Package Worksheet: SBIRT Practice Assessment Tool [PDF - 190 KB] (right) to assess where your team is in implementing SBIRT goals, objectives, and strategies.
- Access the recent IHS Pain and Opioid Use Disorder Webinar recording via Zoom: Overview of New TAPS and CAGE-AID Screening Tools for Substance Use to discover insights on enhancing substance use screening.
- Resource: How to Document Drug and Alcohol Screening and Assessment Tools in the IHS RPMS Electronic Health Record.
TAPS: an online tool administered by the patient or clinician that screens for tobacco, alcohol, illicit drugs and nonmedical use of prescription drugs. It determines a drug-specific risk level.
CAGE-AID: a brief assessment administered by the patient or clinician and has been adapted to include drug use.
Red Lake Nation: Recovery Videos
SUDs disproportionally impact American Indian and Alaska Native people and many communities have developed innovative strategies in response. By sharing stories of community healing we can better understand and serve our relatives that are experiencing SUDs.
- Provider Video: Community Healing - Best Practices
- Patient Video: Sharing Our Stories - Living a Beautiful Life in Recovery (Short Version )
April 2024
Supporting Recovery: Sharing Stories
- An IHS Special General Memorandum (SGM) was released to support the purchase of drug checking equipment.
- The IHS NSSC has a limited amount of xylazine test strips available for order using an IHS-413 form.
Release of Red Lake Nation Recovery Care Videos
Substance use disorders (SUDs) disproportionally impact American Indian and Alaska Native (AI/AN) people and many communities have developed innovative strategies in response. By sharing stories of community healing we can better understand and serve our relatives that are experiencing SUDs. Watch the Red Lake Recovery Videos to learn how local champions came together to heal the community.
Provider Video: Community Healing — Best Practices
The Red Lake Nation’s approach to serving and supporting community members who experience SUD and how they are restoring hope and healing the community. By focusing on a community-based, person- first approach, they save lives and restore families.
- Watch the video Community Healing – Best Practices
Recovery is possible. Hear inspiring recovery stories:
- Watch a Patient Video: Sharing Our Stories - Living a Beautiful Life in Recovery
- Or watch the shortened version
Family Care Plans: Comprehensive Toolkit

Clinicians can impact and improve outcomes for AI/AN Pregnant and Parenting People (PPP) experiencing SUDs. To assist these efforts, the Northwest Portland Area Indian Health Board and HOPE Committee, alongside clinicians and individuals in recovery, developed a Family Care Plans Toolkit .
This toolkit is designed to:
- Help clinicians care for AI/AN PPP and their infants impacted by SUDs
- Support PPP transitioning into and remaining in active recovery
- Assist affected partners and families in growing stronger
NEW TAPS and CAGE-AID Screening Tools for Substance Use Available to Document in IHS RPMS: How-To-Guide now available!
- RPMS How to Guide [PDF - 797 KB]
- TAPS: online tool administered by patient or clinician; screens for: tobacco, alcohol, illicit drugs, nonmedical use of prescription drugs; gives drug-specific risk level.
- CAGE-AID: brief assessment; administered by patient or clinician; adapted to include drug use.
A webinar was hosted in March. Watch the recording.
Team-Based Care: Choosing your Language
Substance use disorder remains to be one of the most stigmatized chronic disease states that continue to impact Indian Country. Health care professionals are often the first point of contact for a person with SUD, professionals should take all steps necessary to reduce the potential for stigma and negative bias. The first step is using non-stigmatizing language. Use person-first language, which maintains the integrity of the individual as a whole human being.
What can you do to reduce stigma?- Be kind and treat those in vulnerable situations with dignity
- Actively listen while someone is sharing their story
- Educate yourself: learn about SUD, how it changes the brain, and how it impacts patients and their families
- Encourage other colleagues to learn more and share what you have learned!
- Avoid labels and replace negative thoughts and assumptions with evidence-based facts
- Change Your Language - Remember, Words Matter!
Newsletter written by HOPE Committee. Contact LCDR Kristin Allmaras with questions.
January 2024
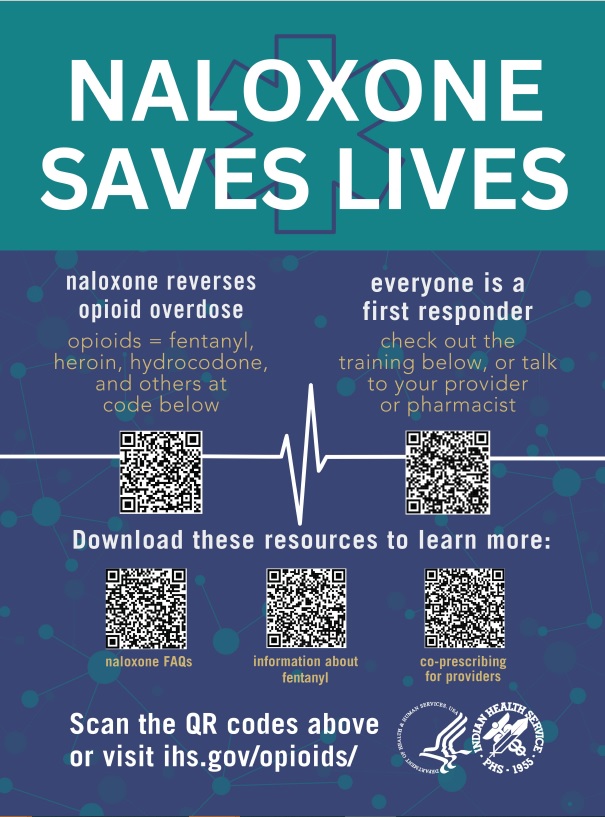
Naloxone: Live-saving Overdose Reversal Medication
Naloxone Keeps the Circle Strong
Naloxone has become a standard first aid tool as a medication that reverses an overdose. It can be given at any time, to anyone. It should be administered even if an opioid overdose is only suspected and not yet confirmed. Studies have shown that community access to naloxone can decrease overdose death rates. IHS has released a variety of resources and tools to support naloxone training in your area:
Naloxone Keeps the Circle Strong Flyer [PDF - 593 KB]
Naloxone Keeps the Circle Strong Guide: How to Start the Naloxone Conversation [PDF - 52 KB]
Virtual, on-demand Naloxone train-the-trainer course
Naloxone Trainings: Consider adapting the training material for your local area!
Naloxone Training for Community Members [PPT - 8 MB]
Naloxone Training for Healthcare Personnel/First Responders [PPT - 11.4 MB]
Naloxone in Schools Toolkit
There is a growing a concern about use of synthetic opioids, such as fentanyl, among our youth. Synthetic opioids cause overdose quickly and can be mixed with other substances, such as marijuana or methamphetamine, without the user’s knowledge. This means that someone’s first use can be fatal if synthetic opioids are present. Schools in many areas have taken action to expand access to overdose prevention efforts. The toolkit provides an example of training plans and materials to support school implementation.
New Naloxone Education Flyers
- Considerations for Co-prescribing Naloxone [PDF - 469 KB]
- FAQs about Naloxone [PDF - 702 KB]
- Opioid Safety Precautions: Fentanyl [PDF - 758 KB]
Contact a naloxone mentor in your IHS Area [PDF - 114 KB] for support with local naloxone initiatives. Mentors can provide an overview of the training materials, program best practices, and offer specific technical assistance.
IHS Educational Outreach Program (EOP): Pain Management Campaign!
EOPs provide frontline clinicians with interactive education, to build relations with healthcare teams, and identify and address system barriers to decrease variability in the use of evidence-based treatments. New clinician guides, pocket-references, fact sheets, and patient education brochures. New clinician guides, pocket-references, fact sheets, and patient education brochures are now available.
Drug Checking Equipment: Test Strips

Fentanyl test strips are now available through the IHS National Supply Service Center (NSSC)
Submit a 413 form to order!
Harm reduction includes individual and community-based safety practices aimed to improve overall health and wellness, with a focus on acceptance instead of abstinence. Basic principles include:
- Valuing all people and their journey by delivering non-judgmental care and education of harm reduction strategies and available services without the fear of shame or punitive action
- Believing that people using substances should be empowered to seek and receive quality healthcare, regardless of their use status
- Recognizing social differences that impact people's ability to change behaviors
Drug checking equipment (such as fentanyl or xylazine test strips) is a strategy to support local harm reduction efforts. They serve as small but vital components of a comprehensive framework to promote health, reduce risk, and engage people struggling with substance use in their own health decisions. For a comprehensive overview of harm reduction pillars, principles, and practices, review SAMHSA’s Harm Reduction Framework. IHS has released a variety of resources to support using drug checking equipment:
- Fentanyl Test Strip Education and Funding
- IHS Harm Reduction Drug Checking Equipment Dispensing Log and facility Policy Examples
State and tribal laws regarding the consideration of FTS as drug paraphernalia may vary. Please consider the implications of these laws in your area prior to product purchasing and deployment.
Syringe Service Programs: The Benefits
Syringe services programs (SSPs) are comprehensive in providing health care and other assistance to persons who use substances. Providing sterile injection equipment and other prevention materials has been shown to reduce the risk of infectious disease transmission, such as HIV and Hepatitis C Virus (HCV) , and reduces needle stick injuries among community members and law enforcement personnel.
Benefits of SSPs:
- Reduce substance use: CDC reports that new users of SSPs are 5 times more likely to enter treatment and 3 times more likely to stop using substances than those who don’t use programs.
- Reduce disease transmission: Data shows a 50% reduction in HIV and HCV incidence with use of SSPs. Transmission is further reduced by over two-thirds when combined with medication-assisted treatment programs. This reduces healthcare costs and the overall burden of disease.
- Improve public safety: A reduction in the number of dirty needles and other used equipment discarded in public areas decreases the risk of disease transmission and needle stick injuries.
- Opioid overdose prevention: Expanded naloxone education and dispensing efforts
- Enhance support: People who participate in SSPs are more likely to openly discuss their needs, likely because they feel empowered to prioritize their health on their own terms. This leads to safer behavioral practices and reduced risk of infections.
IHS hosts sample program documents available for download for anyone interested in starting or expanding local harm reduction efforts.
Newsletter written by HOPE Committee. Contact LCDR Kristin Allmaras with questions.